Common Conditions
Prolapse
Mr Hextall and his team have specialist expertise in treating women with prolapse and see many patients each week with this problem.
Common symptoms include:
- Feeling a lump / swelling in the vagina which may be uncomfortable
- A dragging or dropping sensation
- Backache
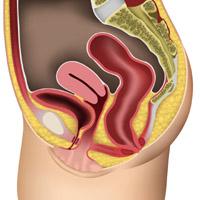
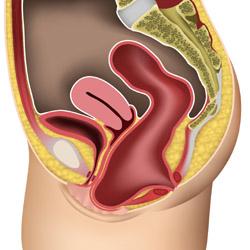
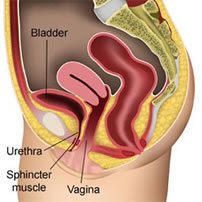 Normal Female Anatomy - no prolapse
Normal Female Anatomy - no prolapse
As the bladder or bowel may prolapse into the vagina, it is quite common for women to develop other symptoms such as incontinence, difficulty emptying and urgency although not everyone is affected in this way. Some patients also find that intercourse is uncomfortable or they don't get enough sensation – the prolapse can also put them off having sex.
Weakness of the vagina along with the surrounding muscles and supports can lead to several different types of prolapse including;
Uterine – prolapse or the uterus / womb
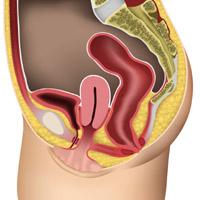
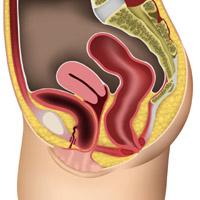
Mild uterine prolapse
the uterus is dropping a little way down into the vagina
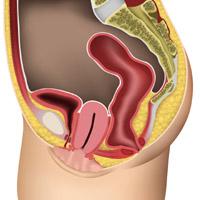
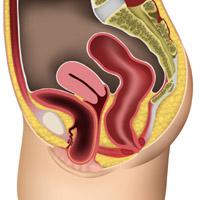
More significant uterine prolapse
The cervix, which is the lowest part of the womb, reaches the vaginal entrance
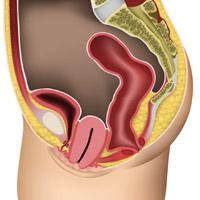
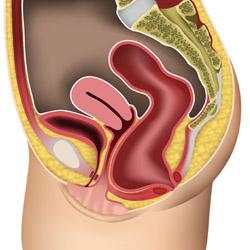
Severe uterine prolapse
The uterus comes right out through the entrance of the vagina
Bladder – also known as a Cystocele
A small cystocele
The bladder is dropping into the vagina
A more significant cystocele
The bladder has dropped and reaches the entrance of the vagina
A severe cystocele
The bladder comes out through the entrance of the vagina
Bowel – also know as Rectocele or Enterocele
A mild rectocele
The bowel is pushing forward or bulging into the vagina
Severe rectocele
The lower bowel (rectum) bulges forward and comes out of the vagina entrance
Vault (top of vagina) – which usually occurs in women who have had a hysterectomy.
No treatment
Not everyone with a prolapse will need treatment. Many women will be found to have a weakness of the vaginal walls or prolapse (perhaps when they have an examination or go for a smear test) and have no symptoms at all. They usually don't require any treatment but should probably try to avoid a lot of heavy lifting or straining as this can make things worse. Pelvic floor exercises may help and these can be taught by Jackie Walker (Urogynaecology Nurse specialist). In addition, we work closely with the physiotherapy teams at Spire Hospital Harpenden, Spire Hospital Bushey and the Redbourn Physiotherapy clinics - redbournphysio.co.uk
Pessaries

Some women prefer to use a pessary – which is a plastic device which sits in the vagina and stops the uterus or walls of the vagina dropping down. This is usually changed every 6 months and is particularly useful for elderly patients or those keen to avoid surgery.
There are several types of pessary but rings are the most common (see picture above). There are several different sizes and once fitted most women feel more comfortable, although they do not suit everyone.
Surgery
The majority of women with a prolapse which is bothering them will choose to have an operation. The type of procedure necessary will obviously depend on the type of prolapse – this will usually be determined by a vaginal examination. Mr Hextall will happy to provide a detailed assessment and performs all surgery himself (in the NHS he also trains junior doctors working towards a Consultant post in gynaecology).
The following information provides a general outline for women who require vaginal surgery for their prolapse.Click here for Vaginal Repair +/- Vaginal Hysterectomy information sheet.
We are also able to offer advanced techniques for women with recurrent problems or those with a prolapse of the top of the vagina (vaginal vault prolapse). Sometimes it is necessary to perform a Sacrocolpopexy procedure which supports the vagina usually a mesh. Click here for Sacrocolpopexy information sheet.
If you would like any further information then please don't hesitate to get in touch.




